

Since OIS is associated with atherosclerosis, patients usually have other related co-morbidities. Other causes include dissecting aneurysm of the carotid artery, giant cell arteritis, fibrovascular dysplasia, Takayasu arteritis, aortic arch syndrome, Behçet’s disease, trauma or inflammation causing stenosis of the carotid arteries and complications after intravitreal anti-VEGF injections and after radiotherapy for nasopharyngeal carcinoma. Ītherosclerosis is the main cause of OIS. In these cases, blood flow is shunted away from the eye to the low-resistance intracranial circuit, with further reduction of retrobulbar blood flow. In patients with OIS, decreased blood flow in the retrobulbar vessels and reversal of blood flow in the ophthalmic artery are found. On the other hand, in patients without well-developed collateral circulation, stenosis of the carotid artery by even 50% may lead to the development of OIS. Patients with well-developed collateral circulation may not develop OIS in spite of total occlusion of the internal carotid artery. OIS occurs mostly in patients with poor collateral circulation between the internal and external carotid arteries or between the two internal carotid arteries. Rarely, the occlusion of the ophthalmic artery is responsible for OIS. It has been estimated that such stenosis reduces the perfusion pressure within the central retinal artery by approximately 50%. In 50% of the cases, the affected artery is completely obstructed. In patients with OIS, a stenosis of 90% or more of the common or internal carotid arteries on the same side is usually found. In this paper we discuss the clinical findings and diagnostic and therapeutic options of ocular ischemic syndrome. It was observed that the signs of ischemia are present in both the anterior and the posterior segments of the eye, and eventually the term ocular ischemic syndrome has been coined for the sum of ocular symptoms and signs that may accompany carotid artery occlusive disease. In the following years, many other terms were introduced to describe ocular changes secondary to carotid artery stenosis, such as ischemic ocular inflammation, ischemic coagulopathy and ischemic ophthalmopathy. They named the condition venous stasis retinopathy and found it in 5% of their patients with unilateral stenosis or occlusion of the internal carotid artery. In the same year, Kearnst and Hollenhorst reported ocular symptoms and signs in association with advanced carotid artery stenosis. He associated these findings with retinal hypoxia due to carotid artery stenosis. In 1963, Hedges described a case of a 48-year-old patient with complete obstruction of the left internal carotid artery on whose eye fundus he observed peripheral blot hemorrhages and dilated retinal veins. Atherosclerosis is the major cause of changes in the carotid arteries. Ocular ischemic syndrome is a rare condition, which is caused by ocular hypoperfusion due to stenosis or occlusion of the common or internal carotid arteries.
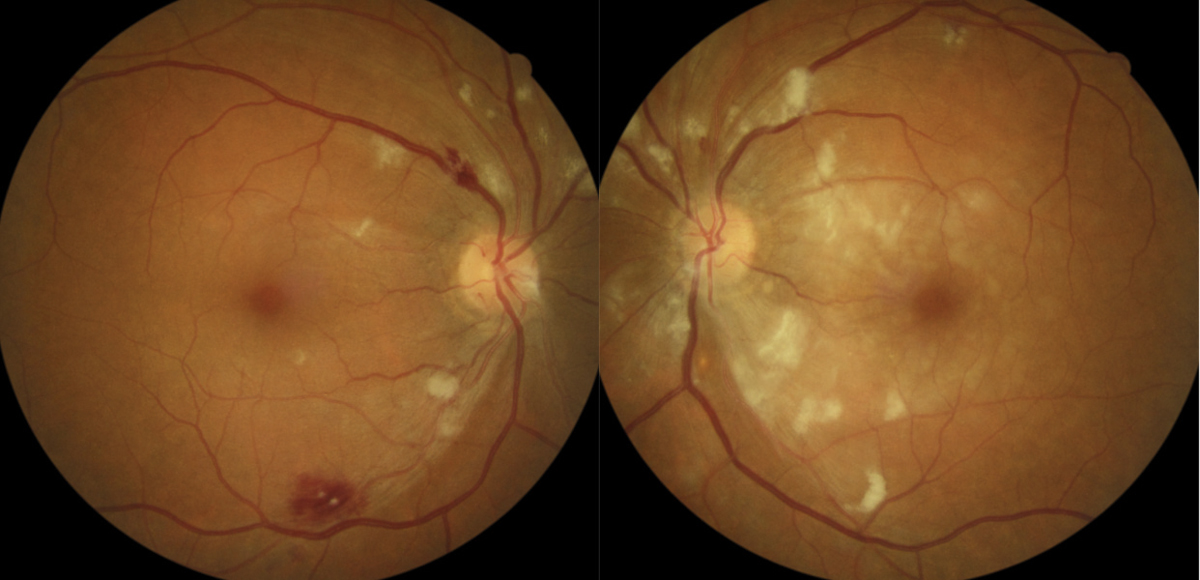
Since the condition does not affect the eyes alone, patients with ocular ischemic syndrome should be referred for consultation to the neurologist, vascular surgeon and cardiologist. The treatment can be local, for example, ocular (conservative, laser and surgical) or systemic (conservative and surgical treatment of the carotid artery). Carotid artery imaging and fundus fluorescein angiography help to establish the diagnosis of ocular ischemic syndrome. Differential diagnosis of ocular ischemic syndrome includes diabetic retinopathy and moderate central retinal vein occlusion. Posterior eye segment changes are the most characteristic, such as narrowed retinal arteries, perifoveal telangiectasias, dilated retinal veins, mid-peripheral retinal hemorrhages, microaneurysms, neovascularization at the optic disk and in the retina, a cherry-red spot, cotton-wool spots, vitreous hemorrhage and normal-tension glaucoma. Anterior segment signs include iris neovascularization and secondary neovascular glaucoma, iridocyclitis, asymmetric cataract, iris atrophy and sluggish reaction to light. Ocular ischemic syndrome is manifested as visual loss, orbital pain and, frequently, changes of the visual field, and various anterior and posterior segment signs.


 0 kommentar(er)
0 kommentar(er)
